Abstract
Background
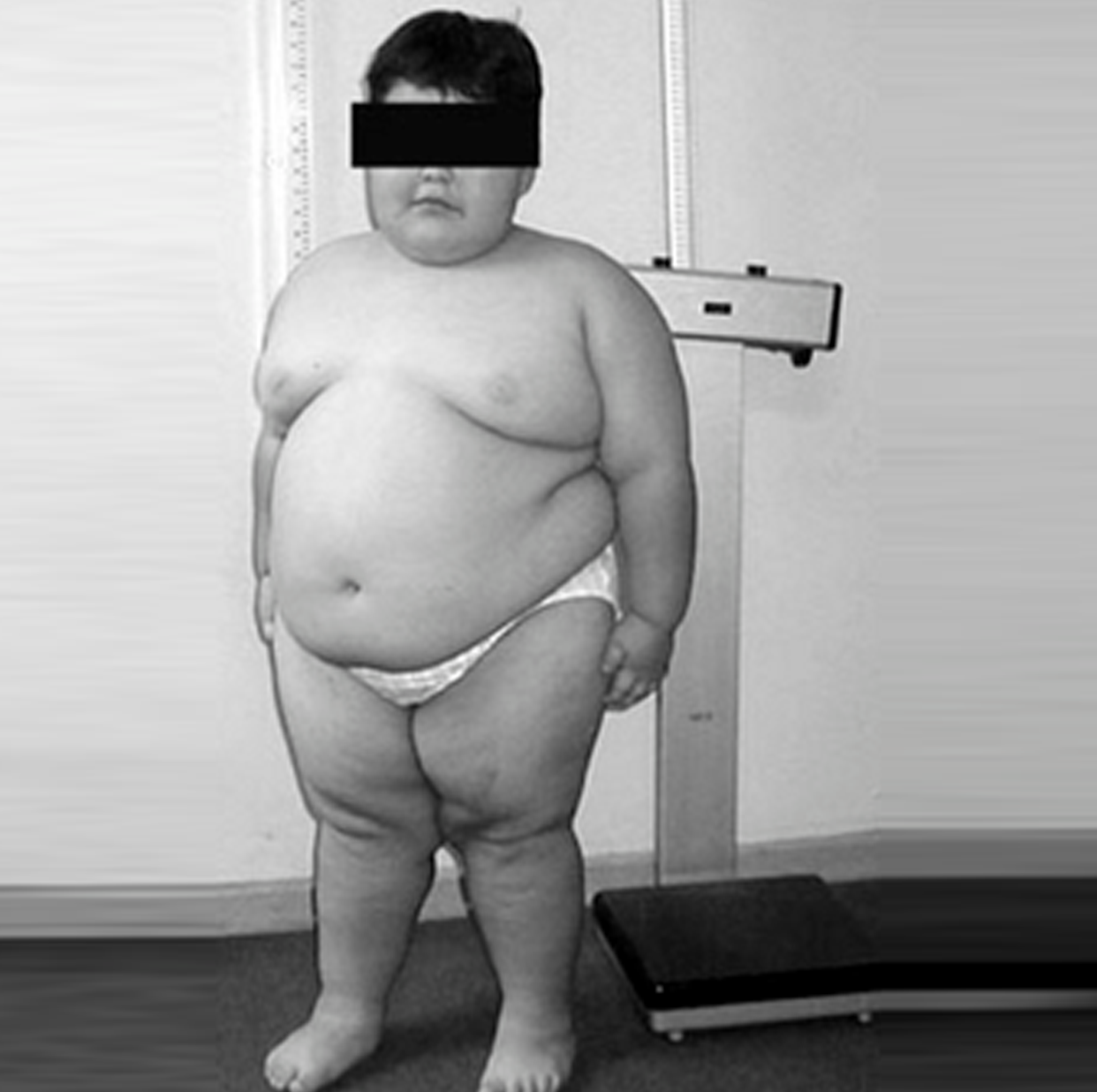
Obesity is a leading cause of mortality and morbidity in Prader-Willi syndrome (PWS).
Objectives
To study weight loss and growth after laparoscopic sleeve gastrectomy (LSG) in pediatric patients with PWS compared with those without the syndrome.
Setting
Academic center with a standardized care pathway for pediatric bariatric surgery as a part of a prospective clinical outcome study on children and adolescents undergoing weight loss surgery.
Methods
Clinical data of all PWS patients who underwent LSG were abstracted from our prospective database, which included all pediatric patients who underwent bariatric surgery. These data were then compared with a 1:3 non-PWS group matched for age, gender, and body mass index (BMI). Data for up to 5 years follow-up were analyzed.
Results
The 24 PWS patients (mean age 10.7; 6<8 yr old, range 4.9–18) had a preoperative BMI of 46.2±12.2 kg/m2. All PWS patients had obstructive sleep apnea (OSA), 62% had dyslipidemia, 43% had hypertension, and 29% had diabetes mellitus. BMI change at the first, second, third, fourth, and fifth annual visits was –14.7 (n = 22 patients), –15.0 (n = 18), 12.2 (n = 13), –12.7 (n = 11), and –10.7 (n = 7), respectively, in the PWS group, whereas the non-PWS group had a BMI change of –15.9 (n = 67), –18.0 (n = 50), –18.4 (n = 47), –18.9 (n = 26), and –19.0 (n = 20), respectively. No significant difference was observed in postoperative BMI change (P = .2–.7) or growth (postoperative height z-score P value at each annual visit = .2–.8); 95% of co-morbidities in both groups were in remission or improved, with no significant difference in the rate of co-morbidity resolution after surgery (P = .73). One PWS patient was readmitted 5 years after surgery with recurrence of OSA and heart failure. No other readmissions occurred, and there were no reoperations, postoperative leaks, or other complications. No mortality or major morbidity was observed during the 5 years of follow-up. Among the PWS patients who reached their follow-up visit time points the total follow-up rate was 94.1%, whereas in the non-PWS group it was 97%. All patients who missed a follow-up visit were subsequently seen in future follow-ups, and no patient was lost to follow-up in either group.
Conclusions
PWS children and adolescents underwent effective weight loss and resolution of co-morbidities after LSG, without mortality, significant morbidity, or slowing of growth. LSG should be offered to obese PWS patients with heightened mortality particularly because no other effective alternative therapy is available.
References:
The study was published in (SURGERY FOR OBESITY AND RELATED DISEASES)

